Author information
- 1Institute of Pharmacology, University of Bern, Bern, Switzerland.
Abstract
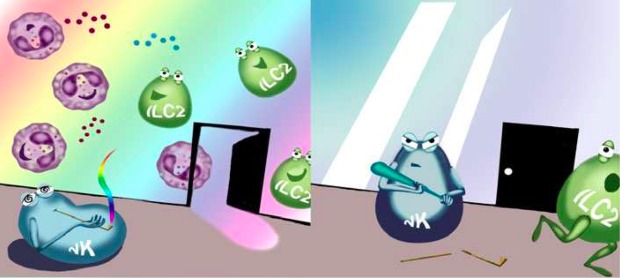
 The network of cells and soluble mediators implicated in the pathogenesis of asthma and allergic disorders is complex. Deciphering details of the crosstalk between its components is essential for the identification of novel drug targets and for advances in patient management and precision medicine (1, 2). There is increasing evidence that innate lymphoid cells (ILCs) contribute to allergic responses (3). This article is protected by copyright. All rights reserved.
The network of cells and soluble mediators implicated in the pathogenesis of asthma and allergic disorders is complex. Deciphering details of the crosstalk between its components is essential for the identification of novel drug targets and for advances in patient management and precision medicine (1, 2). There is increasing evidence that innate lymphoid cells (ILCs) contribute to allergic responses (3). This article is protected by copyright. All rights reserved.
This article is protected by copyright. All rights reserved.
- PMID: 28226397
- DOI: 10.1111/all.13145
- [PubMed – as supplied by publisher]
-
Publication Types
Publication Types

PROF. STEPHAN VON GUNTEN (Orcid ID : 0000-0002-2753-8738)
Received Date : 15-Feb-2017
Accepted Date : 16-Feb-2017
Article type : Editorial
EDITORIAL
(on “CB2 receptors regulate natural killer cells that limit allergic airway inflammation in a murine model of asthma” for Allergy; ref number ALL-2016-00684.R1)Title:
Innate lymphoid cells in asthma: cannabinoids on the balance.
,
(Boligan KF, von Gunten S)
Institute of Pharmacology, University of Bern, Bern, Switzerland
Corresponding author: , MD, PhD, MME, Institute of Pharmacology,University of Bern, INO-F, Inselspital, CH-3013 Bern, Switzerland. Tel.: +41 31 632 32 98;Fax: +41 31 632 49 94; e-mail: stephan.vongunten@pki.unibe.chThis article has been accepted for publication and undergone full peer review but has not been through the copyediting, typesetting, pagination and proofreading process, which may lead to differences between this version and the Version of Record. Please cite this article as doi: 10.1111/all.13145