Revista Brasileira de Psiquiatria
Print version ISSN 1516-4446
Rev. Bras. Psiquiatr. vol.28 no.2 São Paulo June 2006
http://dx.doi.org/10.1590/S1516-44462006000200015
SPECIAL ARTICLE
History of cannabis as a medicine: a review
História da cannabis como medicamento: uma revisão
Antonio Waldo Zuardi
Department of Neurology, Psychiatry and Medical Psychology, Faculdade de Medicina de Ribeirão Preto, Universidade de São Paulo (USP), São Paulo (SP), Brazil
Correspondence
ABSTRACT
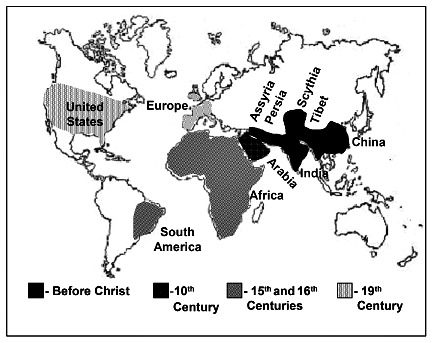
 Cannabis as a medicine was used before the Christian era in Asia, mainly in India. The introduction of cannabis in the Western medicine occurred in the midst of the 19th century, reaching the climax in the last decade of that century, with the availability and usage of cannabis extracts or tinctures. In the first decades of the 20th century, the Western medical use of cannabis significantly decreased largely due to difficulties to obtain consistent results from batches of plant material of different potencies. The identification of the chemical structure of cannabis components and the possibility of obtaining its pure constituents were related to a significant increase in scientific interest in such plant, since 1965. This interest was renewed in the 1990’s with the description of cannabinoid receptors and the identification of an endogenous cannabinoid system in the brain. A new and more consistent cycle of the use of cannabis derivatives as medication begins, since treatment effectiveness and safety started to be scientifically proven.
Cannabis as a medicine was used before the Christian era in Asia, mainly in India. The introduction of cannabis in the Western medicine occurred in the midst of the 19th century, reaching the climax in the last decade of that century, with the availability and usage of cannabis extracts or tinctures. In the first decades of the 20th century, the Western medical use of cannabis significantly decreased largely due to difficulties to obtain consistent results from batches of plant material of different potencies. The identification of the chemical structure of cannabis components and the possibility of obtaining its pure constituents were related to a significant increase in scientific interest in such plant, since 1965. This interest was renewed in the 1990’s with the description of cannabinoid receptors and the identification of an endogenous cannabinoid system in the brain. A new and more consistent cycle of the use of cannabis derivatives as medication begins, since treatment effectiveness and safety started to be scientifically proven.Keywords: Cannabis; Cannabinoids; Tetrahydrocannabinol; History; Therapeutic uses
RESUMO
Antes da Era Cristã, a cannabis foi utilizada na Ásia como medicamento, com grande importância na Índia. A introdução da cannabis na Medicina Ocidental ocorreu em meados do século XIX, atingindo o clímax na última década deste século, com a disponibilidade e o uso de extratos e tinturas da cannabis. Nas primeiras décadas do século XX, o uso médico da cannabis no Ocidente diminuiu significativamente, em grande parte pela dificuldade na obtenção de resultados consistentes de amostras da planta com diferentes potências. A identificação da estrutura química de componentes da cannabis e a possibilidade de se obter seus constituintes puros foram relacionadas a um aumento significativo no interesse científico pela planta, desde 1965. Este interesse foi renovado nos anos 90, com a descrição dos receptores de canabinóides e a identificação de um sistema canabinóide endógeno no cérebro. Usos terapêuticos. Um novo e mais consistente ciclo de uso dos derivados de cannabis como medicamento começa, já que a sua eficácia e segurança no tratamento começam a estar cientificamente provados.
Descritores: Cannabis; Canabinóides; Tetraidrocanabinol; História; Usos terapêuticos
Before the Christian Era
Cannabis Sativa (cannabis) is among the earliest plants cultivated by man. The first evidence of the use of cannabis was found in China, where archeological and historical findings indicate that that plant was cultivated for fibers since 4.000 B.C.1 With the fibers obtained from the cannabis stems, the Chinese manufactured strings, ropes, textiles, and even paper. Textiles and paper made from cannabis were found in the tomb of Emperor Wu (104-87 B.C.), of the Han dynasty.1
The Chinese also used cannabis fruits as food. These fruits are small (3 to 5 mm), elliptic, smooth, with a hard shell, and contain one single seed. The first evidence of the use of these seeds was found during the Han dynasty (206 B.C. – 220 A.D.). In the beginning of the Christian Era, with the introduction of new cultures, cannabis was no longer an important food in China, although, until today, the seeds are still used for making kitchen oil in Nepal.2
The use of cannabis as a medicine by ancient Chinese was reported in the world’s oldest pharmacopoeia, the pen-ts’ao ching which was compiled in the first century of this Era, but based on oral traditions passed down from the time of Emperor Shen-Nung, who lived during the years 2.700 B.C. Indications for the use of cannabis included: rheumatic pain, intestinal constipation, disorders of the female reproductive system, malaria, and others.2 In the beginning of the Christian Era, Hua T’o, the founder of Chinese surgery (A.D. 110 – 207), used a compound of the plant, taken with wine, to anesthetize patients during surgical operations.1
The Chinese used mainly the seeds of cannabis for medical purposes;1 therefore, it may be assumed that they were referring to that part of the plant when describing its medicinal properties. Until today, cannabis seeds continue to be used as a laxative by Chinese physicians.2 It is acknowledged that the seeds are practically deficient in D9-tetrahydrocannabinol (D9-THC), which is considered the plant’s main active constituent, and is mainly composed of essential fatty acids and proteins. Today some of these fatty acids are considered as having therapeutic effects, such as the g-linoleic acid, whose topical use is recommended for eczema and psoriasis, and its oral use for atherosclerosis, osteoporosis, rheumatoid arthritis, and other inflammatory diseases.3 In China, the medical use of cannabis never reached the importance it did in India.
The first reference to the use of cannabis, as a psychoactive drug, is also in the pen-ts’ao ching, as observed in one of its phrases: …ma-fen (the fruit of cannabis)… if taken in excess will produce visions of devils … over a long term, it makes one communicate with spirits and lightens one’s body…4 In spite of this reference, there are scarce citations of the use of cannabis as a hallucinogen in ancient Chinese texts. One possible explanation is that such use was probably associated to shamanism, a religion of the people from Central Asia. During the Han dynasty, this religious practice started to decline in China, and became disbelieved and increasingly restricted. Ancient texts rarely mentioned shamanism and, thus, there is no reference to the use of cannabis as a hallucinogen.2 Although shamanism became gradually more restricted in China, it was rather common in the Northern nomadic tribes, which may have contributed to the dissemination of cannabis in Central and Western Asia and in India.4
In India, the use of cannabis was widely disseminated, both as a medicine and as a recreational drug. Such a broad use may be due to the fact that cannabis maintained a straight association with religion, which assigned sacred virtues to the plant. The Atharva Veda (a collection of sacred texts of unknown author) mentions cannabis as one of five sacred plants, referring to it as a source of happiness, donator of joy and bringer of freedom. Hence, cannabis use became part of numerous religious rituals in that region.2
The plant’s psychoactive effects were well-known in India, possibly due to the way it was prepared for use, which included at least three preparations. The weakest type, Bhang, consists of dry leaves from which flowers are carefully removed. A stronger type, Ganja, is prepared with the female-plant’s flowers. The strongest of them all is the Charas, made exclusively of the resin that covers female flowers.2 These forms of preparation guarantee the presence of active cannabinoids. Currently we know that the plant has secreting hairs that are located mainly on the female-plant’s flowers and, in a smaller amount, on the leaves of its superior third. Solitary resin glands most often form at the tips of the trichome stalks. These glands have a considerable amount of active cannabinoids. Breaking the glands liberates the active cannabinoids.5
In India, the medical and religious use of cannabis probably began together around 1000 years B.C.6 The plant was used for innumerous functions, such as: analgesic (neuralgia, headache, toothache), anticonvulsant (epilepsy, tetanus, rabies), hypnotic, tranquilizer (anxiety, mania, hysteria), anesthetic, anti-inflammatory (rheumatism and other inflammatory diseases), antibiotic (topical use on skin infections, erysipelas, tuberculosis), antiparasite (internal and external worms), antispasmodic (colic, diarrhea), digestive, appetite stimulant, diuretic, aphrodisiac or anaphrodisiac, antitussive and expectorant (bronchitis, asthma).2,6-7
Furthermore, cannabis was traditionally considered sacred in Tibet, although little has been written about its religious or medicinal use. In Tantric Buddhism, which was developed in the Himalayas, cannabis was used to facilitate meditation.2 Though seldom reported, it is believed that the medical use of cannabis in Tibet was intense due to the following reasons: the concepts of Tibetan medicine stem from Hindi medicine; botany was of great importance in its pharmacopoeia; and, finally, cannabis was abundant in that region.2
Evidence suggests that the Assyrians also knew about the psychoactive effects of cannabis and used it as incense since the ninth century B.C.2 It is also possible that, before the Christian Era, Assyrians used the plant externally for swellings and bruises, and internally for depression, impotence, arthritis, kidney stones, ‘female ailment’, and for the ‘annulment of witchcraft’.7
In Persia, cannabis was also known before the Christian Era.6 The Persians knew about the plants biphasic effect, and made a clear distinction between its initial euphoric and its late dysphoric effects.2
In Europe, historical and archeological evidence suggests the presence of cannabis before the Christian Era. It seems the plant was brought by Scythian invaders, who originated from Central Asian and reached close to the Mediterranean. In the year 450 B.C., Herodotus described a Scythian funeral ceremony, and stated that they inhaled the vapors obtained from burning cannabis seeds with ritualistic and euphoric purposes. That description was later confirmed by archeologists who found charred cannabis seeds in Scythian tombs in Siberia and Germany.7
Reference to the use of cannabis by the Greeks and the Romans are scarce, suggesting that it was little used by these people.2,6 In the beginning of the Christian Era, there are two references of the use of the seed’s juice for earache and to drive worms and insects out of the ears.7
Beginning of the Christian Era to the 18th century
In this period, the medical use of cannabis remained very intense in India and was then spread to the Middle East and Africa. In Arabia, well-known physicians mentioned cannabis in their medical compendiums, as Avicena, in the year 1000 A.D.8 Muslim texts mention the use of cannabis as a diuretic, digestive, anti-flatulent, ‘to clean the brain’, and to soothe pain of the ears. In 1464, Ibn al-Badri reported that the epileptic son of the caliph’s chamberlain was treated with the plant’s resin, and stated: it (cannabis) cured him completely, but he became an addict who could not for a moment be without the drug’.7
Cannabis is known in Africa at least since the 15th century, and its use was, possibly, introduced by Arab traders, somehow connected to India. This is evidenced by the similarity of the terms used for preparing the plant in Africa and India. In Africa, the plant was used for snake bite, to facilitate childbirth, malaria, fever, blood poisoning, anthrax, asthma, and dysentery.9
In the Americas, the use of cannabis probably began in South America. In the 16th century, the plant’s seeds reached Brazil; brought by African slaves, especially those from Angola, and its use was considerably common among Blacks in the Northeastern rural area. Most synonyms for cannabis in Brazil (maconha, diamba, liamba, and others) have their origin in the Angolan language. There are reports of the use of cannabis in that region’s popular religious rituals, especially the ‘Catimbó’, which includes cult to African deities and presumes the value of the plant for magical practice and treatment of diseases. In the rural environment, there are reports of the use of cannabis for toothache and menstrual cramps.10
In Europe, during this period, cannabis was cultivated exclusively for fibers. Muslims introduced the manufacture of paper from cannabis, in 1150, first in Spain then in Italy.7 Cannabis descriptions are found in many books about plants written in this period, which clearly state, since the mid 18th century, the distinction between male and female plants (previously described in a Chinese ideogram in the beginning of the Christian Era).7 References to the medical use of cannabis are scarce. Europeans may have known about the plant’s medical use in the Middle East and Africa, but they confused it with opium.7
Western medicine in the 19th and 20th centuries
There are some reports, from the early 19th century, about the use of cannabis by European physicians, especially regarding the use of the seeds or homeopathic medications. However, the effective introduction of cannabis in Western medicine occurred in the midst 19th century through the works of William B. O’Shaughnessy, an Irish physician, and by the book by Jacques-Joseph Moreau, a French psychiatrist.
O’Shaughnessy served in India with the British for several years and made his first contact with cannabis use in that country. He studied the literature on the plant, described many popular preparations, evaluated its toxicity in animals, and, later, he tested its effect on patients with different pathologies. In 1839, he published the work: ‘On the preparations of the Indian hemp, or gunjah‘, which, in the first paragraph, establishes a panorama of plant use:
‘The narcotic effects of Hemp are popularly known in the south of Africa, South America, Turkey, Egypt, Middle East Asia, India, and the adjacent territories of the Malays, Burmese, and Siamese. In all these countries, Hemp is used in various forms, by the dissipated and depraved, as the ready agent of a pleasing intoxication. In the popular medicine of these nations, we find it extensively employed for a multitude of affections. But in Western Europe, its use either as a stimulant or as a remedy is equally unknown’.8
In his book, O’Shaughnessy describes various successful human experiments using cannabis preparations for rheumatism, convulsions, and mainly for muscular spasms of tetanus and rabies.6,8
Moreau used cannabis with a different purpose. He was an assistant physician at the Charenton Asylum, near Paris, and a common therapeutic practice at the time was to accompany psychiatric patients in long trips to exotic and distant countries. During those trips he observed that the use of hashish (cannabis resin) was very common among Arabs, and he was impressed with the substance’s surprising effects. In Paris, around 1840, Moreau decided to experiment, systematically, different cannabis preparations; first on himself and later on his students. As an outcome, in 1845 he published the book ‘Du Hachisch et de l’Alienation Mentale: Etudes Psychologiques‘, with one of the most complete descriptions of the acute effects of cannabis.11 Moreau clearly states his purpose: ‘…I saw in hashish, more specifically in its effects on mental abilities, a powerful and unique method to investigate the genesis of mental illness’.12
These two types of medical interest for cannabis, concerning its psychoactive effects (as an experimental psychotomimetic) as well as its therapeutic use, persisted through the years. O’Shaughnessy and Moreau’s contributions had a great impact on Western medicine, especially due to the scarcity of therapeutic options for infectious diseases such as rabies, cholera, and tetanus. The medical use of the drug spread from England and France reaching all Europe and then North America. In 1860, the first clinical conference about cannabis took place in America, organized by the Ohio State Medical Society.
In the second half of the 19th century, over 100 scientific articles were published in Europe and the United States about the therapeutic value of cannabis.13 The climax of the medical use of cannabis by Western medicine occurred in the late 19th and early 20th century. Various laboratories marketed cannabis extracts or tinctures, such as Merck (Germany), Burroughs-Wellcome (England), Bristol-Meyers Squibb (United States), Parke-Davis (United States), and Eli Lilly (United States).8
The medical indications of cannabis, in the beginning of the 20th century, were summarized in Sajous’s Analytic Cyclopedia of Practical Medicine (1924) in three areas:7
1) Sedative or Hypnotic: in insomnia, senile insomnia, melancholia, mania, delirium tremens, chorea, tetanus, rabies, hay fever, bronchitis, pulmonary tuberculosis, coughs, paralysis agitans, exophtalmic goiter, spasm of the bladder, and gonorrhea.
2) Analgesic: in headaches, migraine, eye-strain, menopause, brain tumors, tic douloureux, neuralgia, gastric ulcer, gastralgia (indigestion), tabes, multiple neuritis, pain not due to lesions, uterine disturbances, dysmenorrhea, chronic inflammation, menorrhagia, impending abortion, postpartum hemorrhage, acute rheumatism, eczema, senile pruritus, tingling, formication and numbness of gout, and for relief of dental pain.
3) Other uses: to improve appetite and digestion, for the ‘pronounced anorexia following exhausting diseases’, gastric neuroses, dyspepsia, diarrhea, dysentery, cholera, nephritis, hematuria, diabetes mellitus, cardiac palpitation, vertigo, sexual atony in the female, and impotence in the male.
Figure 1 shows an illustration of the periods in which the medical uses of cannabis began in different regions.
Decline and rediscovery
In the first decades of the 20th century, the Western medical use of cannabis significantly decreased. This may have occurred, among other factors, because of the difficulty to obtain replicable effects, due to the extreme varying efficacy of different samples of the plant. At that time, the active principle of cannabis had not yet been isolated and the drug was used in the form of tinctures or extracts whose power was dependent on different factors, such as origin, age, and mode of preparation.8 In addition, various medications appeared at the end of the 19th century, with known efficacy for the treatment of the main indications of cannabis. Vaccines were developed for various infectious diseases, such as tetanus; effective analgesics such as aspirin appeared , and hypodermic syringes allowed the injectable use of morphine; and, as a narcotic and sedative, cannabis was rivaled by substances such as chloral hydrate, paraldehyde, and barbiturates.8
Finally, many legal restrictions limited the medical use and experimentation of cannabis. In the United States, as the result of a campaign of the Federal Bureau of Narcotics, the Marihuana Tax Act law was passed in 1937. Under this Act, anyone using the plant was required to register and pay a tax of a dollar an ounce (28.35 g), for medical purposes, and 100 dollars an ounce for any other use. Despite the low value for medical use, the non-payment of this tax, however, resulted in a 2.000 dollar fine and/or 5 years imprisonment. This law brought difficulties for the use of the plant due to the excessive paperwork and the risk of severe punishment. When cannabis transaction regulations, including prescriptions, were transferred to the tribute area, this law circumvented a decision of the Supreme Court which gave the States the right to control commercial transactions and, in practice, meant banning the use of cannabis in the whole American territory. Cannabis was removed from the American pharmacopoeia in 1941.6,14
In the second half of the 20th century, cannabis reached great social importance due to the explosion of its consumption for hedonistic purposes. Until that time, in the West, the hedonistic use of the plant was limited to small groups. In Europe, groups of intellectuals gathered to use the drug. Descriptions of this use may be found in novels by 20th century French writers, such as Gautier and Boudelaire. In the Americas, this practice was relatively common among the Black in the rural area of Northeastern Brazil since the 16th century, who would meet on weekends to use the drug in groups. This use was later passed on to fishermen of the San Francisco River and by sea to the coastal cities. In the early 20th century, the use of cannabis in Brazil remained restricted to small low-socioeconomic groups, and was known as the ‘opium of the poor’.10 In Mexico, cannabis was also used by the most underprivileged population and it was through Mexican immigrants that its use, for recreation, reached the United States in the first decades of the 20th century. Until the 1950’s, in the United States, cannabis use was restricted to the neighborhoods of Blacks and Hispanic immigrants.15
Since the 1960’s, the recreational use of cannabis rapidly spread among the younger ranges of the population throughout the Western world. In the United States, the percentage of young adults that had used cannabis, at least once, went from 5%, in 1967, to 44%, 49%, 68%, and 64%, in 1971, 1975, 1980, and 1982, respectively.16-17 This use remains high until today.18-19 In 1964, the chemical structure of D9-THC was identified by Gaoni and Mechoulam,20 which contributed to a proliferation of studies about the active constituents of cannabis.21
The startling boost in cannabis consumption, which intensified its social importance, along with the better knowledge of its chemical composition (which made it possible to obtain its pure constituents) contributed to a significant increase in scientific interest for cannabis, as of 1965. The number of publications about cannabis reached their peak in the early 1970’s. In this period, a Brazilian research group, led by Carlini, had a great contribution, especially about the interactions of D9-THC with other cannabinoids.22 Since then, Carlini has been developing efforts for the realignment of public policies concerning cannabis control.23 After the middle of 1970’s, the number of publications started to slowly decline during the following two decades. The interest in studies about cannabis was renewed in the early 1990’s, with the description and cloning of specific receptors for the cannabinoids in the nervous system and the subsequent isolation of anandamide, an endogenous cannabinoid.24Afterwards, the number of publications about cannabis has been continuously growing, attesting the great interest in research involving the herb. Figure 2 shows the evolution of the number of publications about cannabis in the last 50 years.
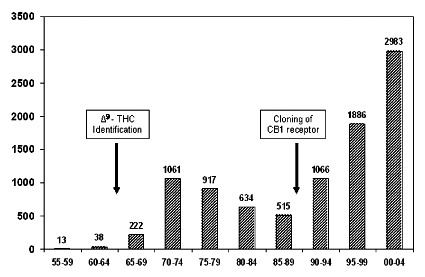
Figure 2 – Number of cannabis-related publications in the last 50 years. The source used was the ‘ISI Web of Knowledge’ with the keywords: cannabis or marijuana or marihuana.
With the growth of scientific interest for cannabis, its therapeutic effects are being once again studied, this time using more accurate scientific methods. There are studies, in different phases, about the therapeutic effects of D9-THC in conditions such as: epilepsy, insomnia, vomits, spasms, pain, glaucoma, asthma, inappetence, Tourette syndrome, and others. Among the therapeutic indications of D9-THC the following are considered close to being proven: anti-emetic, stimulant of appetite, analgesic, and in symptoms of Multiple Sclerosis.25 Other cannabinoids are also under investigation, such as Canabidiol (CBD), which has evidence for therapeutic effects in epilepsy, insomnia, anxiety, inflammations, brain damage (as a neuroprotector), psychoses, and others.26-27 However, cannabis products must be used cautiously since some studies suggest that early-onset cannabis use can induce cognitive deficits and apparently acts as a risk factor for the onset of psychosis among vulnerable youths.28-29
At the beginning of 2005, a multinational pharmaceutical laboratory received the approval in Canada, and is pleading authorization in the United Kingdom and the European Union, to market a medication containing D9-THC and CBD for the relief of neuropathic pain in patients with multiple sclerosis.
Thus, a new cycle begins for the use of cannabis derivatives as medication, this time more consistently than in the past. The structures of chemical compounds derived from cannabis are now known, the mechanisms of their action in the nervous system are being elucidated with the discovery of an endogenous cannabinoid system, and treatment effectiveness and safety are being scientifically proven.
Acknowledgements
Antonio Waldo Zuardi is recipient of National Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) and was supported in part by the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP).
References
1. Li HL, Lin H. An archaeological and historical account of cannabis in China. Econ Bot. 1974;28(4):437-47. [ Links ] 2. Touwn M. The religious and medicinal uses of Cannabis in China, India and Tibet. J Psychoactive Drugs. 1981;13(1):23-34. [ Links ] 3. Leson G, Pless P. Hemp seed and hemp oil. In: Grotenhermen F, Russo E, eds. Cannabis and cannabinoids. New York: The Haworth Integrative Healing Press; 2002. Chapter 38. p. 411-25. [ Links ] 4. Li HL. Hallucinogenic plants in Chinese herbals. J Psychodelic Drugs. 1978;10(1):17-26. [ Links ] 5. Paris M, Nahas GG. Botany: the unstabilizad species. In: Nahas GG, editor. Marihuana in science and medicine. New York: Raven Press; 1984. p. 3-36. [ Links ] 6. Mikuriya TH. Marijuana in medicine: past, present and future. Calif Med. 1969;110(1):34-40. [ Links ] 7. Aldrich M. History of therapeutic cannabis. In: Mathre ML, eds. Cannabis in medical practice. Jefferson, NC: Mc Farland; 1997. p. 35-55. [ Links ] 8. Fankhauser M. History of cannabis in Western Medicine. In: Grotenhermen F, Russo E, eds. Cannabis and Cannabinoids. New York: The Haworth Integrative Healing Press; 2002. Chapter 4. p. 37-51. [ Links ] 9. Du Toit BM. Cannabis in Africa. Rotterdam: Balkema; 1980. [ Links ] 10. Pinho AR. Social and medical aspects of the use of cannabis in Brazil. In: Rubin V, eds. Cannabis and culture.Paris: Mounton Publishers; 1975. p. 293-302. [ Links ] 11. Brill H, Nahas GG. Cannabis intoxication and mental illness. In: Nahas GG, eds. Marihuana in science and medicine. New York: Raven Press; 1984. p. 263-306. [ Links ] 12. Moreau JJ. Du Hachisch et de l’Alienation Mentale: Etudes Psychologiques. Paris: Librarie de Fortin Mason; 1845 (English edition: New York, Raven Press; 1972). [ Links ] 13. Grinspoon L. Marihuana reconsidered. Cambridge, MA: Harvard University Press; 1971. [ Links ] 14. Grinspoon L, Bakalar JB. Marihuana: the forbidden medicine. New Haven: Yale University Press; 1993. Chapter 1. [ Links ] 15. Musto DF. The marihuana tax act of 1937. Arch Gen Psychiatry. 1972;26(2):101-8. [ Links ] 16. Harris LS. Cannabis: a review of progress. In: Lipton MA, Dimascio A, Killam KF, eds. Psychopharmacology: a generation of progress. New York: Raven Press; 1978. p. 1565-74. [ Links ] 17. Kandel DB. Marihuana users in young adulthood. Arch Gen Psychiatry. 1984;41(2):200-9. [ Links ] 18. Department of Health and Human Services. Substance Abuse & Mental Health Services Administration – SAMHSA [cited 2006 Jan 12]. Available from: URL: http://oas.samsa.gov/MJ.htm. [ Links ] 19. European Monitoring Centre for Drugs and Drugs Addiction (EMCDDA) Annual Report 2004: “The state of the drugs problem in the European Union and Norway”. 1-113. Belgium, 2004. [cited 2006 Jan 15]. Available from: URL: http://ar.emcdda.eu.int/pt/home-pt.htm. [ Links ] 20. Gaoni Y, Mechoulam RJ. Isolation structure and partial synthesis of an active constituent of hashish. J Am Chem Soc. 1964;86:1646-7. [ Links ] 21. Mechoulam RJ. Marijuana: chemistry, pharmacology and clinical effects. New York: Academic Press; 1973. p. 2-99. [ Links ] 22. Russo E. A tale of two cannabinoids: the therapeutic rationale for combining tetrahydrocannabinol and cannabidiol. Med Hypotheses. 2006;66(2):234-46. [ Links ] 23. Carlini EA. Conversation with Elisaldo Luiz de Araújo Carlini. Addiction. 2005;100(7):897-907. [ Links ] 24. Martin BR, Mechoulam RJ, Razdan RK. Discovery and characterization of endogenous cannabinoids. Life Sci. 1999;65(6-7):573-95. [ Links ] 25. Carlini EA. The good and bad effects of (-) trans-delta-9- tetrahydrocannabinol (D9-THC) on humans. Toxicon. 2004;44(4):461-7. [ Links ] 26. Mechoulam R, Parker LA, Gallily R. Cannabidiol: an overview of some pharmacological aspects. J Clin Pharmacol. 2002;42(11 Suppl):11S-19S. [ Links ] 27. Zuardi AW, Guimarães FS, Guimarães VM, Del Benl EA. Cannabidiol: possible therapeutic application. In: Grotenhermen F, Russo E, eds. Cannabis and cannabinoids: pharmacology, toxicology and therapeutic potential.New York: The Haword Interactive Healing Press; 2002. Chapter 33. p. 359-69. [ Links ] 28. Pope HG Jr, Gruber AJ, Hudson JI, Cohane G, Huestis MA, Yurgelun-Todd D. Early-onset cannabis use and cognitive deficits: what is the nature of the association? Drug Alcohol Depend. 2003;69(3):303-10. [ Links ] 29. Arseneault L, Cannon M, Witton J, Murray RM. Causal association between cannabis and psychosis: examination of the evidence. Br J Psychiatry. 2004;184:110-7. [ Links ]
 Correspondence
CorrespondenceAntonio Waldo Zuardi
Av. Candido Pereira Lima 745 – Jd. Recreio
14040-250 Ribeirão Preto, SP, Brazil
E-mail: awzuardi@fmrp.usp.br
Submitted: 4 October 2005
Accepted: 21 November 2005
Financing: Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) – Grant 300775/2004-0 and Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP) – Grant 202/13197-2
Conflict of interests: None